Increased MMP9 expression was detected in stenotic and aneurysmal arterial remodeling. As a proinflammatory factor, toll-like receptor 4 upregulates MMP9 expression and mediates inflammatory responses and also contributes to arteriosclerosis. Our previous study has found that T1DMMCAo rats exhibit significantly increased RAGE, TLR4 and MMP9 expression in macrophages in the ischemic brain compared to the ischemic brain of wild-type rats. Generally, smoking, excessive alcohol, untreated hypertension and female gender have been shown to be the most important risk factors for aneurysmal subarachnoid hemorrhage. Recent, large-scale genome-wide association studies have revealed consistent and replicable genetic markers of several complex diseases such as coronary artery disease, and type 2 diabetes may also contribute to IA development. In this study, we investigated the effect of T1DM on IA formation and the underlying mechanism by which T1DM induces IA formation in rats. In this study, to our knowledge we are the first to demonstrate that T1DM promotes the formation of intracranial aneurysm as well as significantly increases RAGE, MMP9 and TLR4 expression in the intracranial arterial wall compared to WT non-DM rats. We also found that T1DM increases cerebral artery IMT and atherosclerosis-like changes identified by decreased arterial diameter and 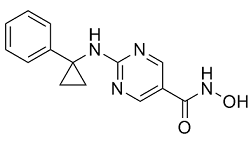 cerebral vascular perfusion, and significantly increases the arterial wall thickness compared to non-DM rats. Previous studies have found that diabetes increases vascular damage and atherosclerotic vascular disease. Consistent with these studies, we found that T1DM significantly increased artery IMT and vascular occlusion and decreased arterial diameter. There are several studies have investigated the effects of abdominal aortic aneurysm formation in diabetic population and demonstrated that diabetes does not aggravate aortic aneurysmal development. However, T1DM significantly increased early stage intracranial aneurysmal formation, but not stage 3 intracranial aneurysmal formation. Our data suggest that T1DM promotes early intracranial aneurism formation, but does not promote aneurysm development to stage 3. The reason for the reduced stage 3 aneurysm development in T1DM is not clear. Possible reasons may be related to: 1) dysregulation of tPA/PAI-1 signaling pathway. A previous clinical report showed that tPA thrombolysis could induce the rupture of cerebral aneurysms. While hyperglycemia significantly increases PAI-1 expression in cerebral arteries and also downregulates t-PA expression and activity, which may increase inflammatory cell accumulation in the lesioned vessels and increase arterial intima-media thickness, and thus attenuates aneurysm diameter, and thereby decreases saccular aneurysm. 2) There may be vascular remodeling after arteriosclerosis in diabetics.
cerebral vascular perfusion, and significantly increases the arterial wall thickness compared to non-DM rats. Previous studies have found that diabetes increases vascular damage and atherosclerotic vascular disease. Consistent with these studies, we found that T1DM significantly increased artery IMT and vascular occlusion and decreased arterial diameter. There are several studies have investigated the effects of abdominal aortic aneurysm formation in diabetic population and demonstrated that diabetes does not aggravate aortic aneurysmal development. However, T1DM significantly increased early stage intracranial aneurysmal formation, but not stage 3 intracranial aneurysmal formation. Our data suggest that T1DM promotes early intracranial aneurism formation, but does not promote aneurysm development to stage 3. The reason for the reduced stage 3 aneurysm development in T1DM is not clear. Possible reasons may be related to: 1) dysregulation of tPA/PAI-1 signaling pathway. A previous clinical report showed that tPA thrombolysis could induce the rupture of cerebral aneurysms. While hyperglycemia significantly increases PAI-1 expression in cerebral arteries and also downregulates t-PA expression and activity, which may increase inflammatory cell accumulation in the lesioned vessels and increase arterial intima-media thickness, and thus attenuates aneurysm diameter, and thereby decreases saccular aneurysm. 2) There may be vascular remodeling after arteriosclerosis in diabetics.
MMP9 degrades the extracellular matrix and is involved in control and regulation of inflammation
Leave a reply